What Are The Primary Causes Of Severs Disease?
Sever's disease (calcaneal apophysitis) is the term used to describe irritation (inflammation) of the calcaneal apophysis. This condition often occurs before or during the growth spurt in boys and girls, or shortly after they begin a new activity. Sever's disease is common is running and jumping sports.
Causes
Sever's disease usually develops as a result of overuse and is common in active children between the ages of 8 to 12. Activities that involve running or jumping can cause undue stress on the calcaneal apophysis. This in turn leads to the development of microscopic damage to the calcaneal apophysis resulting in inflammation and pain. Poor flexibility of the calf muscles and of the Achilles tendon, overpronation (feet rolled in) and inappropriate footwear are some of the other factors that can cause Sever's disease.
Symptoms
The most obvious sign of Sever's disease is pain or tenderness in one or both heels, usually at the back. The pain also might extend to the sides and bottom of the heel, ending near the arch of the foot. A child also may have these related problems, swelling and redness in the heel, difficulty walking, discomfort or stiffness in the feet upon awaking, discomfort when the heel is squeezed on both sides, an unusual walk, such as walking with a limp or on tiptoes to avoid putting pressure on the heel. Symptoms are usually worse during or after activity and get better with rest.
Diagnosis
A doctor or other health professional such as a physiotherapist can diagnose Sever?s disease by asking the young person to describe their symptoms and by conducting a physical examination. In some instances, an x-ray may be necessary to rule out other causes of heel pain, such as heel fractures. Sever?s disease does not show on an x-ray because the damage is in the cartilage.
Non Surgical Treatment
Treatment may consist of one or more of the following. Elevating the heel. Stretching hamstring and calf muscles 2-3 times daily. Using R.I.C.E. (Rest, Ice, Compression, Elevation). Foot orthotics. Medication. Physical therapy. Icing daily (morning). Heating therapy. Open back shoe are best and avoid high heel shoe. The Strickland Protocol has shown a positive response in patients with a mean return to sport in less than 3 weeks. Further research into the anatomical and biomechanical responses of this protocol are currently being undertaken.
Recovery
With proper care, your child should feel better within 2 weeks to 2 months. Your child can start playing sports again only when the heel pain is gone. Your doctor will let you know when physical activity is safe.
Posterior Tibial Tendon Dysfunction
Overview
Adult Acquired Flatfoot occurs when the arch of your foot collapses after your skeleton has stopped growing, usually resulting in the foot ?falling? inward with the toes pointing out. This allows your entire sole to touch the ground when you stand, instead of just the outside area. Arches fall for many reasons, including arthritis, injury to the supporting tendons or bones, nerve problems, diabetic collapse, pregnancy, aging, and obesity. A fallen arch doesn?t have to be painful-though as it develops and worsens, it can lead to strain and weakness in the feet that could allow for more uncomfortable foot problems later. Diabetics can develop serious complications from their fallen arches, and need to have their condition evaluated and treated. 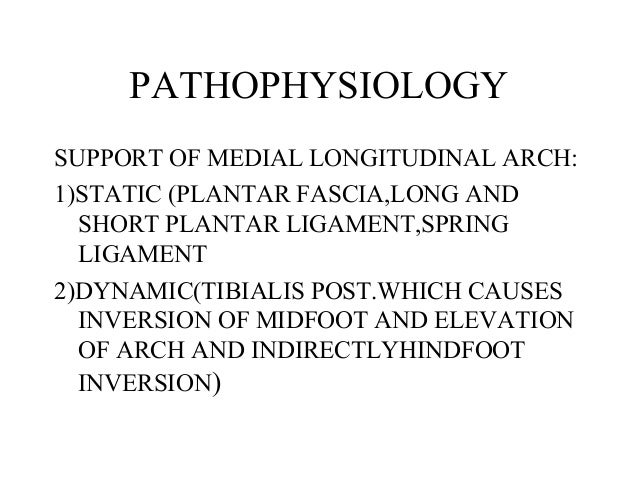
Causes
Flat feet causes greater pressure on the posterior tibial tendon than normal. As the person with flat feet ages, the muscles, tendons and ligaments weaken. Blood supplies diminish as arteries narrow. These conditions are magnified for obese patients because of their increased weight and atherosclerosis. Finally, the tendon gives out or tears. Most of the time, this is a slow process. Once the posterior tibial tendon and ligaments stretch, body weight causes the bones of the arch to move out of position. The foot rotates inward (pronation), the heel bone is tilted to the inside, and the arch appears collapsed. In some cases, the deformity progresses until the foot dislocates outward from the ankle joint.
Symptoms
Pain and swelling behind the inside of your ankle and along your instep. You may be tender behind the inner ankle where the posterior tibial tendon courses and occasionally get burning, shooting, tingling or stabbing pain as a result of inflammation of the nerve inside the tarsal tunnel. Difficulty walking, the inability to walk long distances and a generalised ache while walking even short distances. This may probably become more pronounced at the end of each day. Change in foot shape, sometimes your tendon stretches out, this is due to weakening of the tendon and ligaments. When this occurs, the arch in your foot flattens and a flatfoot deformity occurs, presenting a change in foot shape. Inability to tip-toe, a way of diagnosing Posterior Tibial Tendon Dysfunction is difficulty or inability to ?heel rise? (stand on your toes on one foot). Your tibialis posterior tendon enables you to perform this manoeuvre effectively. You may also experience pain upon attempting to perform a heel rise.
Diagnosis
Starting from the knee down, check for any bowing of the tibia. A tibial varum will cause increased medial stress on the foot and ankle. This is essential to consider in surgical planning. Check the gastrocnemius muscle and Achilles complex via a straight and bent knee check for equinus. If the range of motion improves to at least neutral with bent knee testing of the Achilles complex, one may consider a gastrocnemius recession. If the Achilles complex is still tight with bent knee testing, an Achilles lengthening may be necessary. Check the posterior tibial muscle along its entire course. Palpate the muscle and observe the tendon for strength with a plantarflexion and inversion stress test. Check the flexor muscles for strength in order to see if an adequate transfer tendon is available. Check the anterior tibial tendon for size and strength.
Non surgical Treatment
Treating PTTD is almost always easier the earlier you catch it. So, the first step in treatment is to see your doctor as soon as you begin experiencing painful symptoms. However, once your condition has been diagnosed, your podiatrist will likely try to give the upset tendon a bit of a break so it?ll calm down and stop being so painful. This can often be accomplished by immobilizing the foot using tape and padding, braces, or casts, depending on what your podiatrist believes will work best for you, and depending on the severity of your condition. You may also be instructed to reduce inflammation by applying ice to the area (usually 40 minutes on and 20 minutes off, with a thin towel between you and the ice). Or, you might take anti-inflammatory medications like ibuprofen (steroidal anti-inflammatory meds are actually likely to make this problem worse, and are not usually recommended in treating PTTD), or use ultrasound therapy. Once the inflammation has gone down a bit, your podiatrist may recommend using orthotics (prescription shoe inserts) to support your damaged arch. Ankle braces can also be helpful. 
Surgical Treatment
For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.
Heel Pain And Discomfort Everything You Might Want To Understand Heel Serious Pain

Does your heel feel painful when you get up from bed every morning, or when you get up after sitting down for a long period of time? If you often experience this sort of pain, known as first step pain, you could be suffering from plantar fasciitis (pronounced fash-ee-eye-tus), an inflammation of the plantar fascia, or the band of muscle under the foot. Plantar fasciitis is the most common cause of Heel Pain.
Causes
Achilles tendon rupture, the tendon of the heel cord behind the ankle is torn. Bone bruise. Bone cyst, a solitary fluid-filled cyst (cavity) in a bone. Gout, levels of uric acid in the blood rise until the level becomes excessive (hyperuricemia), causing urate crystals to build up around the joints. This causes inflammation and severe pain when a gout attack happens. Neuroma (Morton's neuroma) a swollen nerve in the ball of the foot, commonly between the base of the second and third toes. Osteomyelitis , osteomyelitis means infection of the bone or bone marrow; inflammation of the bone due to infection. Osteomyelitis sometimes occurs as a complication of injury or surgery. In some cases, the infection may get into bone tissue from the bloodstream. Patients with osteomyelitis typically experience deep pain and muscle spasms in the inflammation area, as well as fever. Peripheral neuropathy, neuropathy is a collection of disorders that occurs when nerves of the peripheral nervous system (the part of the nervous system outside of the brain and spinal cord) are damaged. The condition is generally referred to as peripheral neuropathy, and it is most commonly due to damage to nerve axons. Neuropathy usually causes pain and numbness in the hands and feet. It can result from traumatic injuries, infections, metabolic disorders and exposure to toxins. One of the most common causes of neuropathy is diabetes. Problems with your gait, wrong posture when walking/running. Rheumatoid arthritis, rheumatoid arthritis, sometimes referred to as rheumatoid disease, is a chronic (long lasting), progressive and disabling auto-immune disease condition that causes inflammation and pain in the joints, the tissue around the joints, and other organs in the human body. Rheumatoid arthritis usually affects the joints in the hands and feet first, but any joint may become affected. Patients with rheumatoid arthritis commonly have stiff joints and feel generally unwell and tired.
Symptoms
Usually worse with the first few steps in the morning or at the initial point of activity. The latter usually gets better with continued activity (squeaky hinge analogy). Walking, running, sprinting, hill running and jumping will increase the pain. Often, the natural response is to walk on the outside of the foot - in supination - to lessen the stress on the plantar fascia - resulting in new problems.
Diagnosis
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Orthotics, by treating the cause of the problem, lead to the cure bette than 90% of the time. A small number of patients have waited so long that the plantar fascia has become thickened and filled with scar tissue and are not helped by ?conventional? means. Those are the patients that have, traditionally, required surgical treatment in which the plantar fascia is cut off the heel bone. Luckily, most surgery has been replaced by a relatively new mode of treatment, ESWT or Extracorporeal Shockwave Therapy. ESWT involves the application of multiple shockwaves to the diseased tendon or ligament and has an approximately 85 to 90% success rate. Keep in mind we are talking about this success rate in patients who are ?tough cases,? that is, already had the conventional treatment. The ESWT machines look like miniature renal lithtripsors (kidney stone crushers). There are virtually no side effects to ESWT other than the price as only about 30% of insurance companies are paying for it. They realize that it is less costly and safer than surgery but also know that many more people who would avoid surgery would have no problem getting ESWT so the volume of services would go up. You don?t have to live with painful heels.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
Prevention

It is not always possible to prevent heel pain, but there are measures you can take to help avoid further episodes. Being overweight can place excess pressure and strain on your feet, particularly on your heels. This increases the risk of damaging your feet and heels. If you are overweight, losing weight and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet can be beneficial for your feet. You can calculate your body mass index (BMI) to find out whether you are a healthy weight for your height and build. To work out your BMI, divide your weight in kilograms by your height in metres squared. A BMI of less than 18.5 means that you are underweight, 18.5-24.9 means that your weight is healthy, 25-29 means that you are overweight, 30-40 means that you are obese, over 40 means that you are morbidly obese. You can also use the BMI healthy weight calculator to work out your BMI.
What Are The Main Treatment And Cause Of Achilles Tendinitis Problems ?
 Achilles tendinosis (also known as Achilles tendinopathy) is a soreness and stiffness that comes on gradually and continues to worsen until treated. It is a common injury among middle and long distance runners. The severity of Achilles tendinosis can be broken down into four stages, each of which can be measured in terms of how the Achilles tendon feels during exercise, the amount of stiffness and creaking, and Achilles tendon?s soreness to the touch (the Achilles tendon pinch test). The four stages, or grades, are, No pain during exercise, but there is some discomfort in the morning when first getting out of bed. The stiffness and creaking go away after a few minutes and are fine the rest of the day. Lightly pinching the Achilles tendon with the forefinger and thumb in the morning or after exercise will probably indicate soreness. Pain during exercise or running, but performance is not affected. The stiffness and creaking continue to appear when first getting out of bed and continue to disappear shortly afterward. Lightly pinching the Achilles tendon with the forefinger and thumb in the morning or after exercise will indicate soreness. Pain during exercise or running that is detrimental to performance. The stiffness and creaking continue to appear when first getting out of bed, but may continue for some time and reappear at other points during the day. Lightly pinching the Achilles tendon with the forefinger and thumb in the morning or after exercise will indicate soreness. Hurts too much to exercise or run. The stiffness and creaking continue to appear when first getting out of bed, but may continue for most of the day. Lightly pinching the Achilles tendon with the forefinger and thumb at almost any time of day will indicate soreness.
Achilles tendinosis (also known as Achilles tendinopathy) is a soreness and stiffness that comes on gradually and continues to worsen until treated. It is a common injury among middle and long distance runners. The severity of Achilles tendinosis can be broken down into four stages, each of which can be measured in terms of how the Achilles tendon feels during exercise, the amount of stiffness and creaking, and Achilles tendon?s soreness to the touch (the Achilles tendon pinch test). The four stages, or grades, are, No pain during exercise, but there is some discomfort in the morning when first getting out of bed. The stiffness and creaking go away after a few minutes and are fine the rest of the day. Lightly pinching the Achilles tendon with the forefinger and thumb in the morning or after exercise will probably indicate soreness. Pain during exercise or running, but performance is not affected. The stiffness and creaking continue to appear when first getting out of bed and continue to disappear shortly afterward. Lightly pinching the Achilles tendon with the forefinger and thumb in the morning or after exercise will indicate soreness. Pain during exercise or running that is detrimental to performance. The stiffness and creaking continue to appear when first getting out of bed, but may continue for some time and reappear at other points during the day. Lightly pinching the Achilles tendon with the forefinger and thumb in the morning or after exercise will indicate soreness. Hurts too much to exercise or run. The stiffness and creaking continue to appear when first getting out of bed, but may continue for most of the day. Lightly pinching the Achilles tendon with the forefinger and thumb at almost any time of day will indicate soreness.
Causes
Unusual use or overuse of the lower leg muscles and Achilles tendon is usually the cause of Achilles tendinitis. Repetitive jumping, kicking, and sprinting can lead to Achilles tendinitis in both recreational and competitive athletes. Runners, dancers, and athletes over age 65 are especially at risk. Sudden increases in training or competition can also inflame your Achilles tendon. For example, adding hills, stair-climbing, or sprinting to your running workout puts extra stress on your Achilles tendon. Improper technique during training can also strain the tendon. Intense running or jumping without stretching and strengthening your lower leg muscles can put you at risk regardless of your age or fitness level. Running on tight, exhausted, or fatigued calf muscles can put added stress on your Achilles tendon, as your tendon may not be ready to quickly start a workout after a period of inactivity. Direct blows or other injuries to the ankle, foot, or lower leg may pull your Achilles tendon too far and stretch the tissue. A hard contraction of the calf muscles, such as can happen when you push for the final sprint in a race, can strain the tendon. People whose feet roll inward, a condition called overpronation, are particularly at risk. Sometimes, shoes with too much heel cushioning put extra strain on the Achilles tendon.
Symptoms
Symptoms include pain in the heel and along the tendon when walking or running. The area may feel painful and stiff in the morning. The tendon may be painful to touch or move. The area may be swollen and warm. You may have trouble standing up on one toe.
Diagnosis
X-rays are usually normal in patients with Achilles tendonitis, but are performed to evaluate for other possible conditions. Occasionally, an MRI is needed to evaluate a patient for tears within the tendon. If there is a thought of surgical treatment an MRI may be helpful for preoperative evaluation and planning.
Nonsurgical Treatment
Relieving the stress is the first course of action. Treatment involves ice therapy and activity modification to reduce inflamation. Active stretching and strengthening exercises will assist rehabilitation of the gastrocnemius-soleus complex. When placed in a heeled shoe, the patient will immediately notice a difference, compared to flat ground. It is recommended that the patient be fitted with proper shoes & orthotics to control pronation and maintain proper alignment, relieving the stress on the achilles tendon. Tightness in the tendon itself can be helped by an extra heel lift added to the orthotics. The patient can expect a slow recovery over a period of months.

Surgical Treatment
Occasionally, conservative management of Achilles tendon conditions fails. This failure is more common in older male patients and those with longstanding symptoms, those who persist in full training despite symptoms or those who have uncorrected predisposing factors. In these cases, surgery may be indicated. It should be remembered, however, that the rehabilitation program, particularly for severe Achilles tendon injuries, is a slow, lengthy program. Surgery is only indicated when there is failure to progress in the rehabilitation program. Surgery should not be considered unless at least six months of appropriate conservative management has failed to lead to improvement.
Prevention
You can take measures to reduce your risk of developing Achilles Tendinitis. This includes, Increasing your activity level gradually, choosing your shoes carefully, daily stretching and doing exercises to strengthen your calf muscles. As well, applying a small amount ZAX?s Original Heelspur Cream onto your Achilles tendon before and after exercise.
What Is Heel Discomfort
Overview
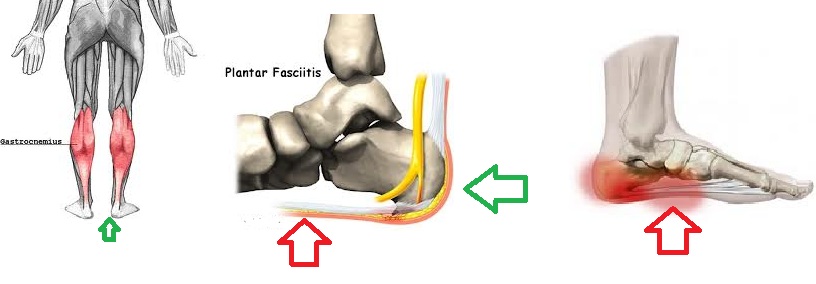
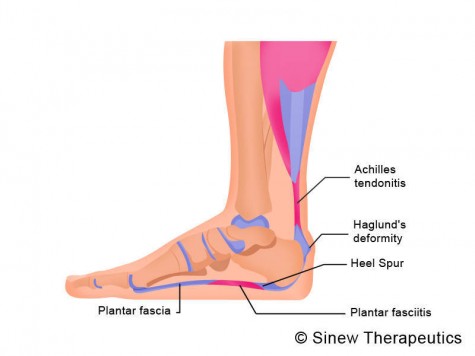
Plantar fasciitis is one of the most common explanations of heel pain. It is caused by inflammation to the thick band that connects the toes to the heel bone, called the plantar fascia, which runs across the bottom of your foot. The condition is most commonly seen in runners, pregnant women, overweight people, and individuals who wear inadequately supporting shoes. Plantar fasciitis typically affects people between the ages of 40 and 70.
Causes
Far and away the most common cause of plantar fasciitis in an athlete is faulty biomechanics of the foot or leg. Faulty biomechanics causes the foot to sustain increased or prolonged stresses over and above those of routine ground contacts. Throughout the phase of ground contact, the foot assumes several mechanical positions to dissipate shock while at the same time placing the foot in the best position to deliver ground forces. With heel landing the foot is supinated (ankle rolled out). At mid-stance the foot is pronated (ankle rolled in). The foot is supinated again with toe-off. The supination of the foot at heel strike and toe-off makes the foot a rigid lever. At heel strike the shock of ground contact is transferred to the powerful quads. During toe-off forward motion is created by contraction of the gastroc complex plantar flexing the rigid lever of the foot pushing the body forward.
Symptoms
Plantar fasciitis is the inflammation of the plantar fascia - a band of tough fibrous tissue running along the sole of the foot. It occurs when small tears develop in the plantar fascia, leading to inflammation and heel pain. The plantar fascia tissue branches out from the heel like a fan, connecting the heel bone to the base of the toes. When the foot moves, the plantar fascia stretches and contracts. The plantar fascia helps to maintain the arch of the foot in much the same way that the string of a bow maintains the bow's arch. The most notable symptom of plantar fasciitis is heel pain. This is typically most severe in the middle of the heel though it may radiate along the sole of the foot. The pain is most often felt when walking first thing in the morning or after a period of rest. As walking continues the pain may decrease; however some degree of pain remains present on movement. The pain may disappear when resting, as the plantar fascia is relaxed. Redness, swelling and warmth over the affected area may also be noticed. The onset of plantar fasciitis is gradual and only mild pain may be experienced initially. However, as the condition progresses the pain experienced tends to become more severe. Chronic plantar fasciitis may cause a person to change their walking or running action, leading to symptoms of discomfort in the knee, hip and back.
Diagnosis
Your doctor can usually diagnose plantar fasciitis just by talking to you and examining your feet. Rarely, tests are needed if the diagnosis is uncertain or to rule out other possible causes of heel pain. These can include X-rays of the heel or an ultrasound scan of the fascia. An ultrasound scan usually shows thickening and swelling of the fascia in plantar fasciitis.
Non Surgical Treatment
Treatment for plantar fasciitis should begin with rest, icing, and over the counter medications. As mentioned above, an orthotic is a device that can be slipped into any pair of shoes and can often relieve pain and help to reverse the damage and occurrence of plantar fasciitis. They do this by adding support to the heel and helping to distribute weight during movement. In addition to orthotics, many people consider night splints for treating this condition. These devices are worn during the night while you sleep, helping to keep the plantar fascia stretched to promote healing. Physical therapy has also become a common option. With this conservative treatment alternative, a physical therapist designs a set of exercises that are intended to address your specific needs in order to promote healing.

Surgical Treatment
Like every surgical procedure, plantar fasciitis surgery carries some risks. Because of these risks your doctor will probably advise you to continue with the conventional treatments at least 6 months before giving you approval for surgery. Some health experts recommend home treatment as long as 12 months. If you can’t work because of your heel pain, can’t perform your everyday activities or your athletic career is in danger, you may consider a plantar fasciitis surgery earlier. But keep in mind that there is no guarantee that the pain will go away completely after surgery. Surgery is effective in many cases, however, 20 to 25 percent of patients continue to experience heel pain after having a plantar fasciitis surgery.
What Causes Heel Discomfort And How To Prevent It

Overview
Plantar fasciitis, also called “heel pain syndrome,” affects approximately 2 million people in the United States each year. Plantar fasciitis can come on gradually as the result of a degenerative process or sudden foot trauma. It can appear in one heel or both. It is generally worse on taking the first few steps in the morning or after prolonged sitting or non-weight-bearing movement. Symptoms can be aggravated by activity and prolonged weight bearing. Obesity, too, is hard on the feet-it can cause plantar pain or it can make that pain worse. The plantar fascia connects the calcaneal tubercle to the forefoot with five slips directed to each toe respectively. Other conditions, such as calcaneal fat pad atrophy, calcaneal stress fracture, nerve entrapment, and rheumatoid arthritis may also cause foot pain. These conditions may be found in combination with plantar fasciitis, or separate from it. A blood test can help pinpoint the cause(s).
Causes
When some people stand/walk/run/jump their own anatomy in their ankle joint is not ‘sturdy’ enough to cope with the needed stabilisation of their ankle joint when they are weight bearing. So, their ankle rotates to find a point of stability. By the shin twisting in and the ankle rotating downwards to the inside (along with your body weight, the power of some muscles, and of course, gravity) a huge amount of stress is applied to the plantar fascia until it is stressed beyond it’s normal limits and it starts to ‘tighten up’. It is this tightening up of the plantar fascia under this stress that causes the damage that in turn leads to pain…eventually.
Symptoms
Plantar fasciitis has a few possible symptoms. The symptoms can occur suddenly or gradually. Not all of the symptoms must be present at once. The classic symptom of plantar fasciitis is pain around the heel with the first few steps out of bed or after resting for a considerable period of time. This pain fades away a few minutes after the feet warm up. This symptom is so common that it symbols the plantar fasciitis disorder. If you have it then probably you have plantar fasciitis. If you don’t suffer from morning pain then you might want to reconsider your diagnosis. Pain below the heel bone at the connection of the bone to the fascia. As the condition becomes more severe the pain can get more intense during the day without rest. Plantar fasciitis symptoms include pain while touching the inside of the heel or along the arch. Foot pain after you spend long periods of time standing on your feet. Pain when stretching the plantar fascia. Foot pain that worsens when climbing stairs or standing on the toes. Pain that feels as though you are walking on glass. Pain when you start to exercise that gets better as you warm up but returns after you stop.
Diagnosis
Plantar fasciosis is confirmed if firm thumb pressure applied to the calcaneus when the foot is dorsiflexed elicits pain. Fascial pain along the plantar medial border of the fascia may also be present. If findings are equivocal, demonstration of a heel spur on x-ray may support the diagnosis; however, absence does not rule out the diagnosis, and visible spurs are not generally the cause of symptoms. Also, infrequently, calcaneal spurs appear ill defined on x-ray, exhibiting fluffy new bone formation, suggesting spondyloarthropathy (eg, ankylosing spondylitis, reactive arthritis. If an acute fascial tear is suspected, MRI is done.
Non Surgical Treatment
Orthotics are corrective foot devices. They are not the same as soft, spongy, rubber footbeds, gel heel cups etc. Gel and rubber footbeds may cushion the heels and feet, but they do not provide any biomechanical correction. In fact, gel can do the opposite and make an incorrect walking pattern even more unstable! Orthotic insoles work by supporting the arches while re-aligning the ankles and lower legs. Most people’s arches look quite normal when sitting or even standing. However, when putting weight on the foot the arches lower, placing added tension on the plantar fascia, leading to inflammation at the heel bone. Orthotics support the arches, which reduces the tension and overwork of the plantar fascia, allowing the inflamed tissue to heal. Orthotics needn’t be expensive, custom-made devices. A comprehensive Heel Pain study by the American Orthopaedic Foot and Ankle Society found that by wearing standard orthotics and doing a number of daily exercises, 95% of patients experienced substantial, lasting relief from their heel pain symptoms.
Surgical Treatment
Surgery may be considered in very difficult cases. Surgery is usually only advised if your pain has not eased after 12 months despite other treatments. The operation involves separating your plantar fascia from where it connects to the bone; this is called a plantar fascia release. It may also involve removal of a spur on the calcaneum if one is present. Surgery is not always successful. It can cause complications in some people so it should be considered as a last resort. Complications may include infection, increased pain, injury to nearby nerves, or rupture of the plantar fascia.
What Is Heel Discomfort

Overview
Plantar fasciitis causes pain in the bottom of the heel. The plantar fascia is a thin ligament that connects your heel to the front of your foot. It supports the arch in your foot and is important in helping you walk. Plantar fasciitis is one of the most common orthopedic complaints. Your plantar fascia ligaments experience a lot of wear and tear in your daily life. Normally, these ligaments act as shock absorbers, supporting the arch of the foot. Too much pressure on your feet can damage or tear the ligaments. The plantar fascia becomes inflamed, and the inflammation causes heel pain and stiffness.
Causes
Plantar fasciitis generally occurs over time, rather than being the result of a single event. Micro trauma from repetitive stress to the tissue often combines with a biomechanical deficiency of the foot to produce the condition. In addition, arthritic and metabolic factors may contribute to the development of this injury, (though they are unlikely to affect young athletes). A variety of training errors commonly lead to plantar fasciitis, particularly a rapid increase in either volume or intensity of athletic activity. Volume refers to the distance or time an athlete performs, while intensity refers to the pace of activity and/or the recovery time allowed following performance.
Symptoms
Symptoms of the plantar fasciitis include a gradual onset of pain under the heel which may radiate into the foot. Tenderness is usually felt under and on the inside of the heel which is initially worse first in the morning but eases as the foot warms up only to return later in the day or after exercise. Stretching the plantar fascia may be painful.
Diagnosis
Plantar fasciosis is confirmed if firm thumb pressure applied to the calcaneus when the foot is dorsiflexed elicits pain. Fascial pain along the plantar medial border of the fascia may also be present. If findings are equivocal, demonstration of a heel spur on x-ray may support the diagnosis; however, absence does not rule out the diagnosis, and visible spurs are not generally the cause of symptoms. Also, infrequently, calcaneal spurs appear ill defined on x-ray, exhibiting fluffy new bone formation, suggesting spondyloarthropathy (eg, ankylosing spondylitis, reactive arthritis. If an acute fascial tear is suspected, MRI is done.
Non Surgical Treatment
Conservative treatment is almost always successful, given enough time. Traditional treatment often includes, rest, NSAIDs, and new shoes or heel inserts. Some doctors also recommend avoiding walking bare-footed. This means you’d have to wear your shoes as soon as you wake up. Certain foot and calf exercises are often prescribed to slowly build strength in the ligaments and muscles that support the arch of the foot. While traditional treatment usually relieves pain, it can last from several months to 2 years before symptoms get better. On average, non-Airrosti patients tend to get better in about 9 months.

Surgical Treatment
More invasive procedures to treat plantar fasciitis are usually sought only after other treatment has failed to produce favorable results. Corticosteroid injections deliver medicine into the injured fascia to reduce pain. However, this treatment may weaken the plantar fascia and result in further damage. In addition, extracorporeal shock wave therapy (ESWT) is a treatment where sound waves are sent through the damaged tissue in order to stimulate the damaged tissue and encourage healing. This method is relatively new in treating plantar fasciitis and your doctor will be able to tell you if it is the right method for you. Lastly, surgery is the last option for those suffering from chronic or severe plantar fasciitis.